I’m an Assistant Professor in the Divisions of Cardiothoracic Anesthesiology, Clinical and Translational Research (DoCTR), and Institute for Informatics (I2) at the Washington University School of Medicine in St Louis. My research is focused on the use of clinical informatics and data science to improve clinician workflow, efficiency, and the quality of clinical care.
- Clinical Informatics
- Electronic Health Record Optimization
- Perioperative Blood Management
- Machine Learning for Healthcare
Fellowship in Adult Cardiothoracic Anesthesiology, 2022
Washington University in St Louis
Residency in Anesthesiology, 2022
Washington University in St Louis
MD, PhD in Systems Biology, 2017
Stanford University
Featured Publications
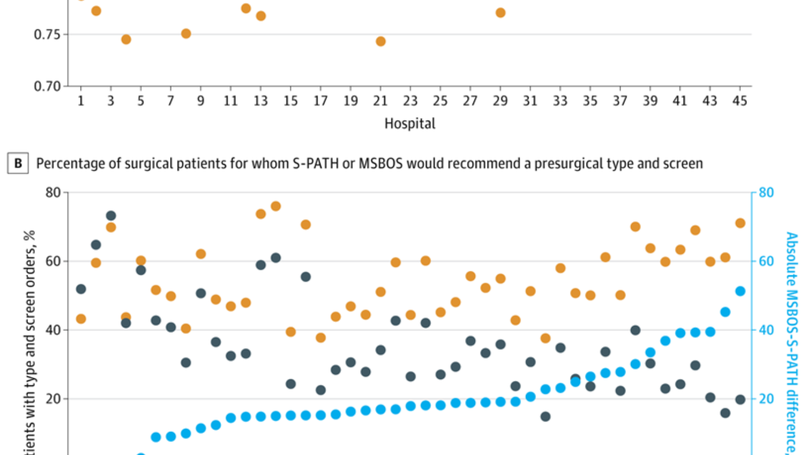
We previously developed a personalized AI model to predict surgical transfusion risk. Here we simulated using it for preop T&S decisions at 45 US hospitals. Our model (S-PATH) did better than the standard of care approach (MSBOS). We also measured performance using a clinically meaningful benchmark, the number of T&S ordered. S-PATH needed ~ 1/3 fewer while maintaining 96% sensitivity for finding patients who need blood. Importantly, we used S-PATH out of the box. No retraining or fine tuning on individual hospitals. Nonetheless, it still performed well. This kind of robustness is rare among AI models, and suggests S-PATH could be immediately useful for many hospital systems.
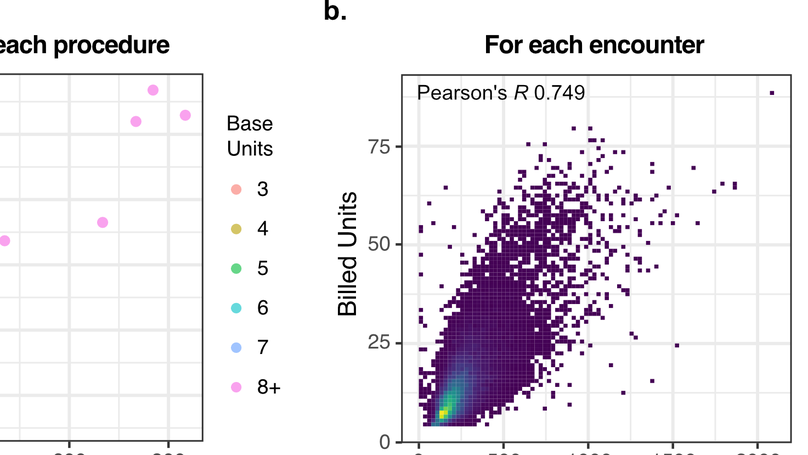
We compared EHR-based workload with reimbursement in anesthesiology and found that payments for anesthesia services are likely poorly calibrated with clinical workload, largely by not recognizing the physical and cognitive effort of caring for the sickest patients. This likely penalizes academic and safety net hospitals the most. Our method for measuring clinical workload from EHR audit log data could be used to measure the time and intensity of clinical work more objectively to better inform healthcare policy.
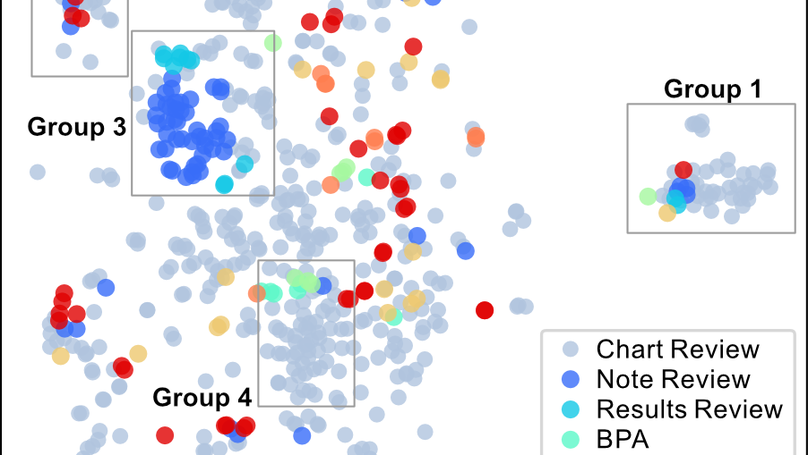
Audit logs have great potential for studying the EHR-based workflows and work habits of physicians and other healthcare professionals. However, one major barrier is the granularity of the data, which makes identification of discrete clinical tasks difficult. In this paper, we describe a novel unsupervised approach using the comparison and visualization of EHR action embeddings to learn context and structure from raw audit log activities, which can be useful for task identification and annotation.
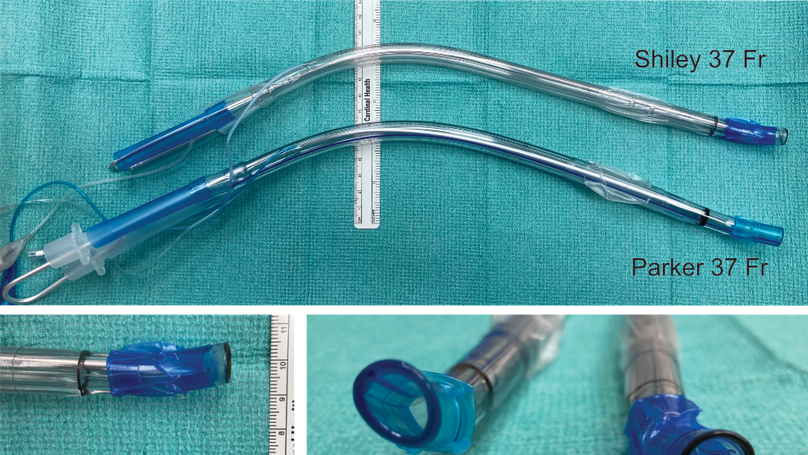
Double lumen tube (DLT) sizes can vary considerably between manufacturers. This can lead to inadvertent oversizing of DLTs, especially if using conventional height/gender based sizing, which can potentially contribute to tracheal injury. We advocate for CT based sizing of DLTs, especially in high risk patients, and for thermal softening of DLTs as routine practice to help prevent tracheobronchial injury.
Recent Publications
Contact
- [first letter of first name][last name]@wustl.edu
- One Barnes Jewish Hospital Plaza, St Louis, MO 63110













