Abstract
Background Clinical environments are characterized by competing demands for patient care, communication, and documentation, thus requiring clinicians to constantly switch their attention between multiple tasks. The objective of this study is to assess the consequences of electronic health record (EHR)-based attention switching on workload and wrong-patient errors for intensive care unit (ICU) clinicians.
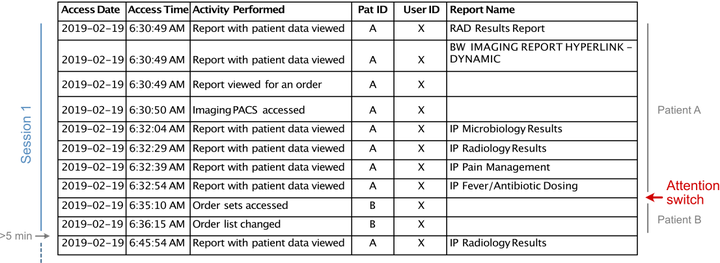
Methods We conducted a retrospective cohort study using EHR-based audit logs—traces of clinician actions—for ICU attending physicians and advanced practice providers (APPs). Attention switching was defined as any transition from one patient’s chart to another within an uninterrupted single session of EHR use. Total EHR time per shift was used as a measure of EHR-based workload. Retract-and-reorder events were used as a measure of wrong-patient errors. Association between attention switching and EHR-based workload was assessed using linear mixed-effect models, and that between attention switching and wrong-patient errors was assessed using a Poisson regression.
Results There were 62,367 hours of EHR use during the study period. EHR-based work was fragmented, with frequent attention switching between patients (median=57/shift for attendings, 60 for APPs). Attention switching was associated with increased EHR-based workload for APPs [β=0.28 for an increase from 4.0 (25th percentile) to 8.6 (75th percentile) switches per 100 EHR actions, 95% CI 0.24-0.32], but not for attending physicians. Attention switching was associated with an increased risk for wrong-patient errors [rate ratio=1.25, for an increase from 25th to 75th percentile, 95% CI 1.03-1.47].
Conclusions Attention switching is common among ICU clinicians and has direct implications for clinician workload and patient safety.