Temporal Associations Between EHR-Derived Workload, Burnout, and Errors; a Prospective Cohort Study
Abstract
Background The temporal progression and workload-related causal contributors to physician burnout are not well-understood.
Objective To characterize burnout’s time course and evaluate the effect of time-varying workload on burnout and medical errors.
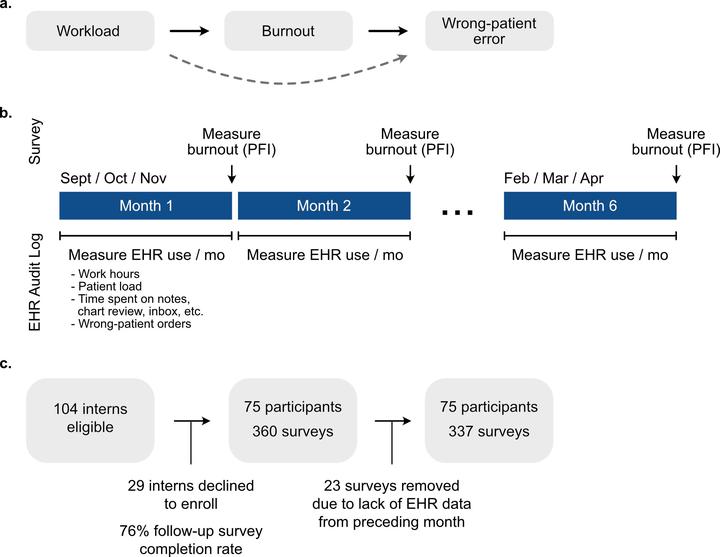
Design Six-month longitudinal cohort study with measurements of burnout, workload, and wrong-patient orders every 4 weeks.
Participants Seventy-five intern physicians in internal medicine, pediatrics, and anesthesiology at a large academic medical center.
Main Measures Burnout was measured using the Professional Fulfillment Index survey. Workload was collected from electronic health record (EHR) audit logs and summarized as follows, total time spent on the EHR, after-hours EHR time, patient load, inbox time, chart review time, note-writing time, and number of orders. Wrong-patient orders were assessed using retract-and-reorder events.
Results Seventy-five of 104 interns enrolled (72.1%) in the study. A total of 337 surveys and 8,863,318 EHR-based actions were analyzed. Median burnout score across the cohort across all time points was 1.2 (IQR 0.7-1.7). Individual-level burnout was variable (median monthly change 0.3, IQR 0.1-0.6). In multivariable analysis, increased total EHR time (β=0.121 for an increase from 54.5 h per month (25th percentile) to 123.0 h per month (75th percentile), 95%CI=0.016-0.226), increased patient load (β=0.130 for an increase from 4.9 (25th percentile) to 7.1 (75th percentile) patients per day, 95%CI=0.053-0.207), and increased chart review time (β=0.096 for an increase from 0.39 (25th percentile) to 0.59 (75th percentile) hours per patient per day, 95%CI=0.015-0.177) were associated with an increased burnout score. After adjusting for the total number of ordering sessions, burnout was not statistically associated with an increased rate of wrong-patient orders (rate ratio=1.20, 95%CI=0.76-1.89).
Conclusions Burnout and recovery were associated with recent clinical workload for a cohort of physician trainees, highlighting the elastic nature of burnout. Wellness interventions should focus on strategies to mitigate sustained elevations of work responsibilities.